Myelinated nerve fibers.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

Myelinated nerve fibers.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

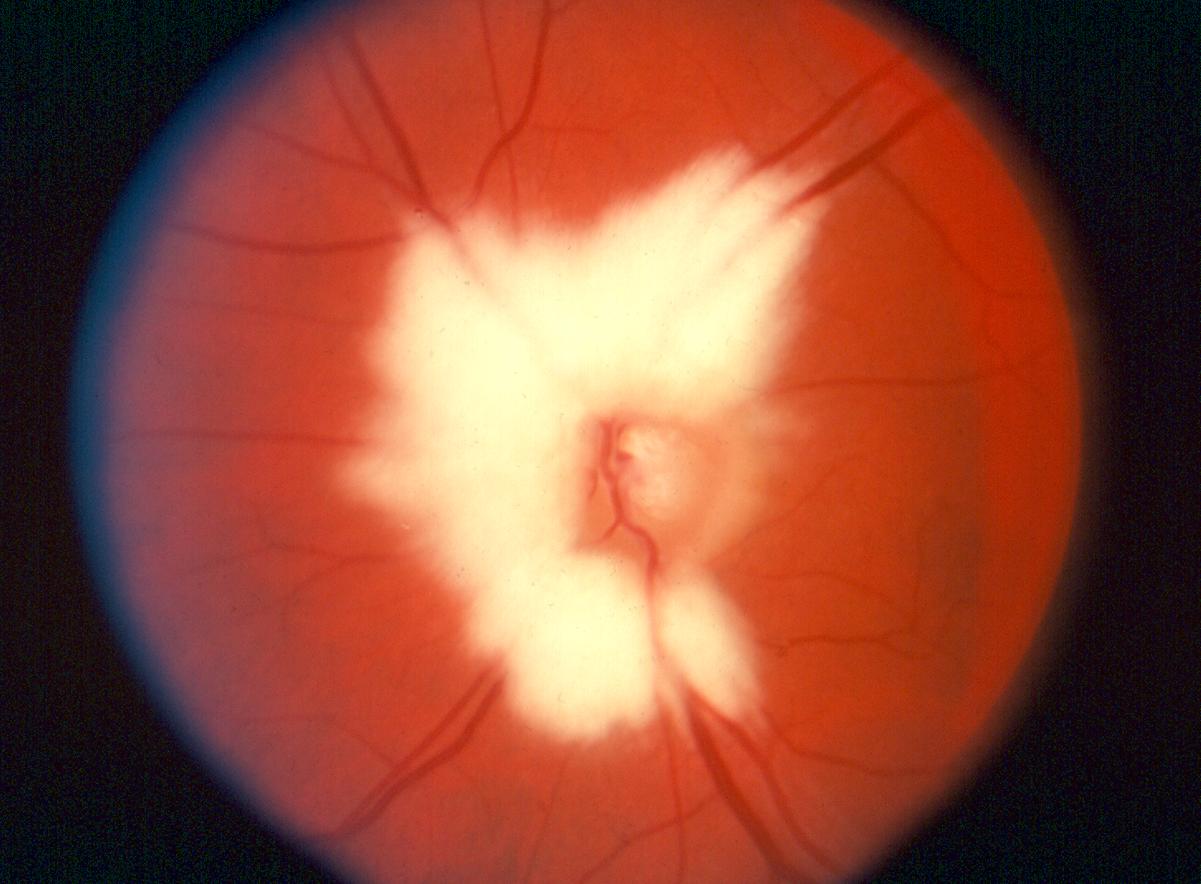
Myelinated nerve fibers
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

Myelinated nerve fibers.
Image credit: Courtesy of Rod Foroozan, M.D. American Academy of Ophthalmology. Used with permission for educational purposes.

Myelinated nerve fibers.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.
Myelinated nerve fibers.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

Myelinated nerve fibers.
Image credit: Courtesy of Andre Marques, M.D. American Academy of Ophthalmology. Used with permission for educational purposes.

Myelinated nerve fibers.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

Optic disc drusen.
Image credit: Courtesy of Andre Marques, M.D. American Academy of Ophthalmology. Used with permission for educational purposes.

Optic disc drusen.
Image credit: Courtesy of Rod Foroozan, M.D. American Academy of Ophthalmology. Used with permission for education purposes.

Optic disc drusen.
Image credit: Courtesy of Mansi Parikh, M.D. American Academy of Ophthalmology. Used with permission for educational purposes.

Buried optic disc drusen.
A. Left optic disc demonstrating fullness but no obvious drusen.
B. B-scan ultrasonography of patient’s left eye reveals hyperechoic, high signal characteristic of optic disc drusen (see arrow).
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

Optic disc drusen.
Optic disc drusen are hyaline or calcified deposits within the optic nerve head. They may be visible at the optic nerve head or buried. Nasal visual field defects and other glaucoma-like visual field defects may be present, though most visual field defects are asymptomatic.
There are many imaging modalities that help visualize optic nerve drusen, including B-scan ultrasonography (C), autofluorescence (D), and CT (E).
A. Fundus photograph of optic disc drusen, showing blurred disc margin with scalloped edge, refractile bodies on the disc surface and at the superior pole, mild pallor, and no obscuration of retinal blood vessels.
B. Visual field patterns confirmed the presence of a nasal step produced by drusen involving the right disc.
C. B-scan ultrasonogram, demonstrating focal, highly reflective (due to calcification) elevation within the optic disc (arrow), which persists when the gain is decreased
D. Preinjection fundus photograph demonstrating autofluorescence (arrow).
E. CT scan of the orbits. Calcified optic disc drusen are visible bilaterally at the posterior globe–optic nerve junction (arrows).
Part A courtesy of Steven A. Newman, MD; part B courtesy of Michael S. Lee, MD; parts C, E courtesy of Anthony C. Arnold, MD; part D courtesy of Hal Shaw, MD.
Image credit: Basic and Clinical Science Course, Section 5: Neuro-Ophthalmology. San Francisco: American Academy of Ophthalmology, 2018-2019: 142. Used with permission for educational purposes.

Optic disc drusen.
Optic disc drusen are hyaline and calcified nodules within the optic nerve head. They may be visible on the surface of the optic nerve or buried, mimicking optic nerve edema (pseudoedema). Drusen may autofluoresce, which may help reveal optic disc drusen.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

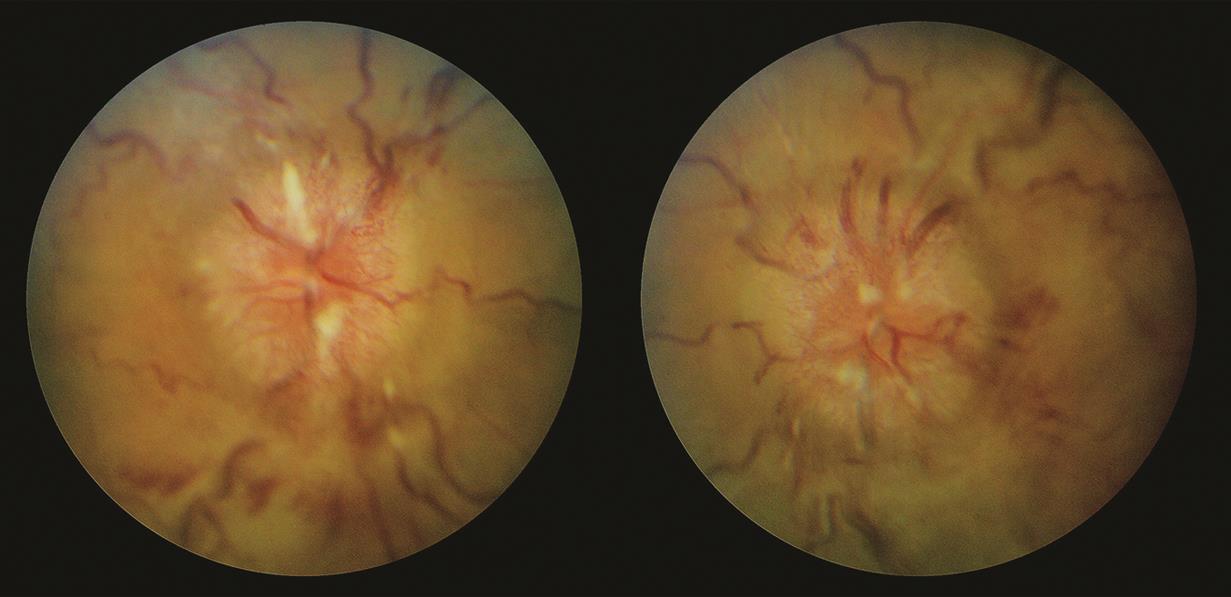
Chronic papilledema from superior sagittal sinus thrombosis.
In the right eye, the optic nerve is diffusely elevated with nerve fiber layer edema. There is some mild tortuosity to the retinal vessels, and the smaller retinal vessels are obscured at the margins of the optic nerve. This is characteristic of Frisén grade 3 papilledema. Just temporal to the optic nerve are very faint dark lines concentric to the optic nerve. These are retinal folds (Paton lines), which can be seen in papilledema.
In the left eye, the optic nerve is diffusely elevated with nerve fiber layer edema. There is also some mild tortuosity, but the retinal vessels do not appear obscured by the nerve fiber layer edema. This is characteristic of Frisén grade 2 papilledema.
Because idiopathic intracranial hypertension is a diagnosis of exclusion, all patients with suspected papilledema need to be worked up for secondary causes of intracranial hypertension with an MRI ± MRV brain, lumbar puncture with opening pressure, and cerebrospinal fluid (CSF) studies.
Image credit: Schiefer, Wilhelm, Hart (Eds.). Clinical Neuro-Ophthalmology - A Practical Guide. Springer: Berlin/Heidelberg/New York, 2007. Used for educational purposes.
Very severe papilledema.
In the right eye, there is diffuse elevation of the optic nerve with nerve fiber layer edema. The optic nerve is hyperemic with cotton-wool infarcts, most prominently at the superior and inferior poles of the optic nerve. There are multiple flame (splinter) hemorrhages throughout the posterior pole. There are telangiectatic vessels on the optic nerve. The retinal vessels are tortuous. The retinal vessels at the optic nerve are not clearly visible at all. This is characteristic of Frisén grade 5 papilledema.
The left eye has similar descriptive features and also has Frisén grade 5 papilledema.
This case of papilledema was secondary to tetracycline use. Treatment of pseudotumor cerebri secondary to drug use after confirmation of the diagnosis includes discontinuation of the offending drug and conventional treatment for intracranial hypertension, which may include observation, weight loss, medical therapy, and/or surgical therapy. Other medications that have association with pseudotumor cerebri include other tetracyclines (minocycline, doxycycline), vitamin A toxicity (>100,000 IU/day), all-trans retinoic acid (ATRA), Accutane, synthetic growth hormone, lithium, and steroid use/withdrawal.
Image credit: American Academy of Ophthalmology. Used with permission for educational purposes.

Severe papilledema.
The optic nerve is diffusely elevated with nerve fiber layer edema present 360°. The optic nerve is diffusely hyperemic and there are telangiectatic vessels on the surface of the nerve. There is a flame (splinter) hemorrhage on the temporal aspect of the optic nerve. The retinal vessels are dilated and tortuous, suggestive of venous congestion. The smaller retinal vessels are partially obscured at the edge of the optic nerve but the larger central retinal vessels are still visible. This is characteristic of Frisén grade 3 papilledema.
On an unrelated note, if you look carefully at the pattern of white striae in the retina you can see the different bundles of nerve fibers (arcuate, papillomacular, and nasal) as they course from the retina to the optic nerve.
Image credit: FitzGibbon EJ. EyeWiki. American Academy of Ophthalmology. Accessed 04-11-2019. Available online. Used with permission for educational purposes.

Moderate papilledema.
The optic nerve is diffusely elevated with involvement of the entire optic nerve. The optic nerve is hyperemic. Some of the retinal vasculature is tortuous. There are no telangiectatic vessels, cotton-wool spots, or hemorrhages. There are no retinal or choroidal folds. The retinal vessels are still clearly visible. This appearance is characteristic of Frisén grade 2 papilledema.
Image credit: FitzGibbon EJ. EyeWiki. American Academy of Ophthalmology. Accessed 04-11-2019. Available online. Used with permission for educational purposes.

Mild papilledema.
The margins of the optic nerve are still visible but there is nerve fiber layer edema (whitish feathery halo) more prominently seen superiorly, inferiorly, and nasally. There are no hemorrhages or cotton-wool spots. The retinal vasculature is intact and visible. There are no choroidal or retinal folds. Because the temporal margin of the optic nerve is still intact, this would fall in the category of Frisén grade 1 papilledema.
Image credit: FitzGibbon EJ. EyeWiki. American Academy of Ophthalmology. Accessed 04-11-2019. Available online. Used with permission for educational purposes.

Papilledema in pseudotumor cerebri.
The right eye demonstrates diffuse nerve fiber layer edema (white feathery appearance) and there is diffuse elevation of the optic nerve. Telangiectatic vessels lie on the surface of the optic nerve (one more prominently seen temporally). The major retinal vessels are obscured by the thickened nerve fiber layer centrally but not completely obliterated by the edema. There are no obvious retinal or choroidal folds. This is characteristic of Frisén grade 4 papilledema.
The left eye demonstrates diffuse nerve fiber layer edema with diffuse elevation of the optic nerve. The disc is hyperemic and there are no obvious telangiectatic vessels. Nasally, there is a thin and faint whitish vertical/circumferential line that most likely indicates the extent of subretinal fluid emanating from the optic nerve. Some of the smaller retinal vessels are obscured by the thickened nerve fiber layer, but the largest retinal vessels remain completely visible. This is characteristic of Frisén grade 3 papilledema.
Image credit: Hoyt WF. Bilateral papilledema with pseudotumor cerebri. Neuro-Ophthalmology Virtual Education Library. University of Utah, 2012. Available online. Used for educational purposes.

B-scan ultrasound in papilledema.
A. Diameter of the optic nerve sheath in a normal person.
B. Diameter of the optic nerve sheath in a patient with IIH.
C. Diameter of the optic nerve sheath in the same patient as (B) following lumbar puncture with therapeutic removal of CSF.
Image credit: Bäuerle J, Nedelmann M. B-mode sonography of the optic nerve in neurological disorders with altered intracranial pressure. Perspectives in Medicine 2012;1:404-407. Available online.