To help increase the amount of helpful study content on this site, I’ve partnered with some medical students from East Tennessee State University! They are being mentored by one of my former ophthalmology residents, Dr. Brent Aebi. The posts are primarily authored by the medical student, and reviewed/edited by myself and Dr. Aebi.
This post and one-page coffee table book excerpt about Retinopathy of Prematurity was written by Ansam Qaddoumi, B.S., B.A.
Research and text by Ansam Qaddoumi, B.S., B.A.
Editing by Brent E. Aebi, M.D. and Kevin E. Lai, M.D.
Formatting by Ansam Qaddoumi, B.S., B.A.. and Kevin E. Lai, M.D.
All image sources cited in document. Created in Canva.
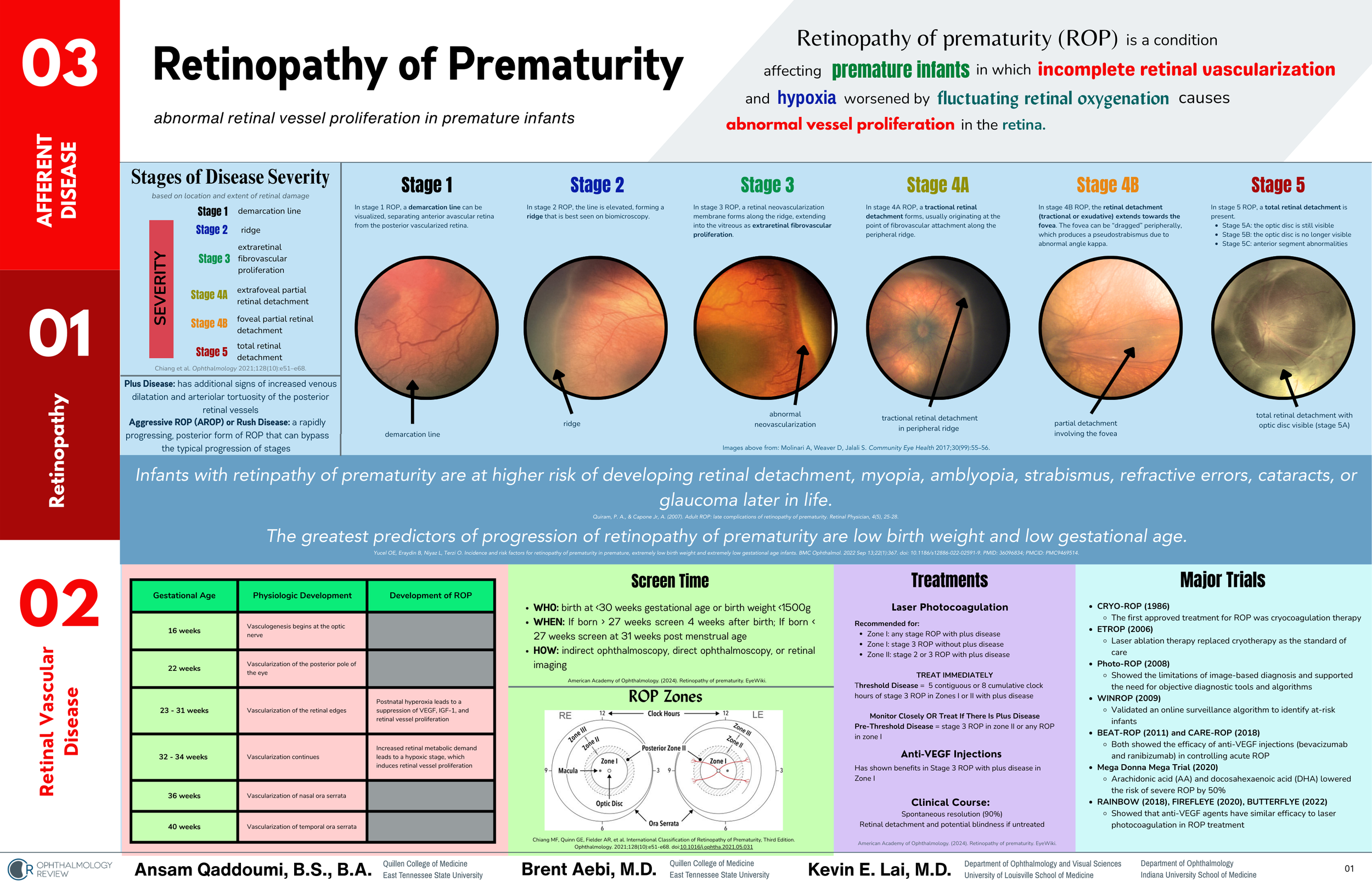
Retinopathy of prematurity (ROP) is a vasoproliferative disorder that affects the retinas of premature infants which is caused by a combination of incomplete vascularization of the developing retina and supplemental oxygen damage to the retina.
Pathophysiology
Normal Gestational Development
During normal gestation, vasculogenesis of the retina usually starts around 16 weeks of gestational age (GA), beginning at the optic nerve and spreading outwards. By 22 weeks, the posterior pole of the eye becomes vascularized. Between 23-31 weeks, vasculogenesis continues until it has spread to the edges of the retina. Finally, the nasal ora serrata becomes vascularized by 36 weeks GA and the temporal ora serrata is fully vascularized by 40 weeks GA.
What Happens to the Retina in Premature Infants
For infants who are born prematurely, this process is disrupted before the retina is completely vascularized. In infants who are born before 32 weeks GA, the postnatal exposure to excessive oxygen leads to a suppression of VEGF, IGF-1, and retinal vessel proliferation. Next, between 32-34 weeks GA, the increased retinal metabolic demand leads to a relatively hypoxic state, which then induces excessive retinal vessel proliferation.
This creates a mismatch between the vascular needs of the retina and the high levels of oxygen that many premature infants receive. There are two phases in the pathophysiologic development of ROP. Phase 1 is a hyperoxic state which suppresses both VEGF production and retinal vascular growth. Phase 2 is a hypoxic state which then induces neovascularization as the metabolic demand of the retina increases.
Classification
The nomenclature of ROP is standardized to facilitate clinical identification, management decisions, and research worldwide. The International Classification of Retinopathy of Prematurity (ICROP) details these terms and is periodically updated to reflect advances in this condition.
There are five (5) sets of classifications for ROP:
Location (zone)
Vessel appearance (“plus” disease)
Severity (stage)
Extent
Progression
Combined, these descriptions form the framework by which we determine treatment protocols, evaluate progression (or improvement), and follow-up intervals.
When we describe ROP in an eye, we must describe all five components. For example, a Zone II, Stage 1 Plus involving 3 clock-hours without aggressive features is managed differently than a Zone III, Stage 1, no Plus involving 2 clock-hours without aggressive features.
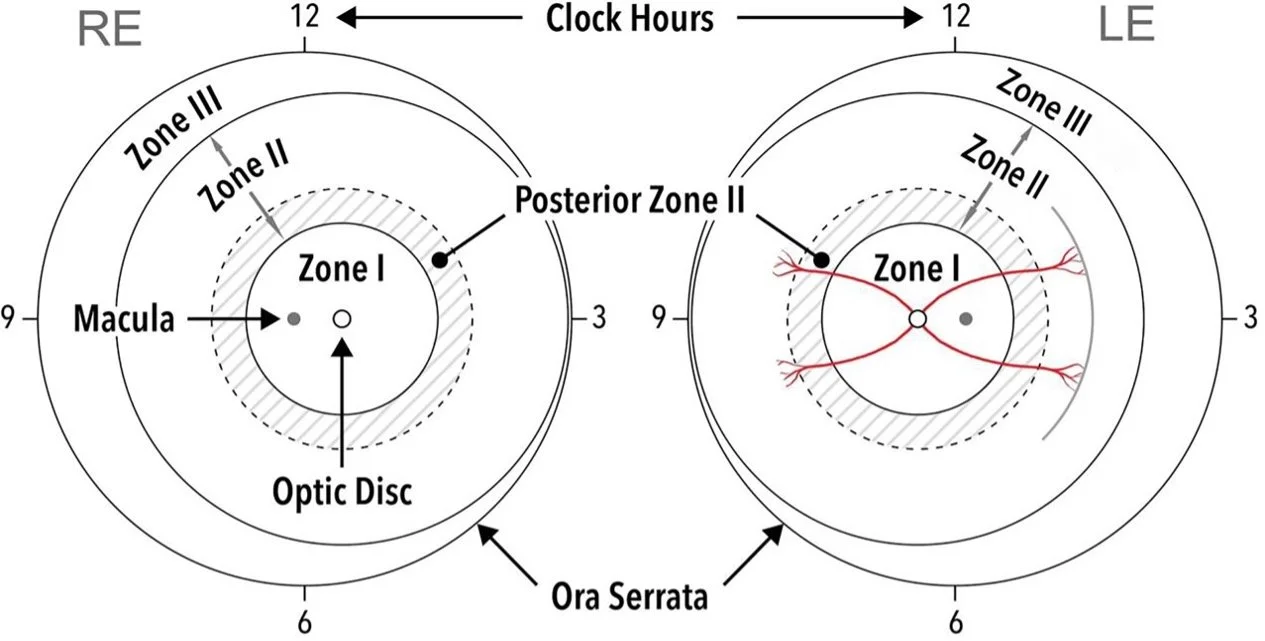
Location (Zones)
Figure 1: Zone borders and clock hours per ICROP3.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, Binenbaum G, Blair M, Peter Campbell J, Capone A Jr, Chen Y, Dai S, Ells A, Fleck BW, Good WV, Elizabeth Hartnett M, Holmstrom G, Kusaka S, Kychenthal A, Lepore D, Lorenz B, Martinez-Castellanos MA, Özdek Ş, Ademola-Popoola D, Reynolds JD, Shah PK, Shapiro M, Stahl A, Toth C, Vinekar A, Visser L, Wallace DK, Wu WC, Zhao P, Zin A. International Classification of Retinopathy of Prematurity, Third Edition. Ophthalmology. 2021 Oct;128(10):e51-e68. doi: 10.1016/j.ophtha.2021.05.031. Epub 2021 Jul 8. PMID: 34247850; PMCID: PMC10979521.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10979521/
Reproduced for educational purposes.
Zone I
Zone I represents a circle with a radius that is twice the distance from the optic disc to the fovea.
Zone II
Zone II starts from the edge of Zone I and extends to the nasal ora serrata. Posterior Zone II is a region of 2-disc diameters peripheral to Zone I. ROP in posterior zone II usually indicates more aggressive disease.
Zone III
Zone III refers to the residual crescent of peripheral retina that extends beyond Zone II.
Vessel Appearance (“Plus” Disease)
Plus disease is a spectrum to describe the extent of more severe disease characterized by signs of increased venous dilatation and arteriolar tortuosity in the posterior retina. Per ICROP3 criteria, there should be at least 2 quadrants with vascular dilatation and tortuosity to be considered plus disease. Pre-plus disease indicates that there are more vascular abnormalities in the posterior retina than normal but not enough to classify for plus disease.
Figure 2: Plus disease spectrum per ICROP3.
Chiang MF, Quinn GE, Fielder AR, Ostmo SR, Paul Chan RV, Berrocal A, Binenbaum G, Blair M, Peter Campbell J, Capone A Jr, Chen Y, Dai S, Ells A, Fleck BW, Good WV, Elizabeth Hartnett M, Holmstrom G, Kusaka S, Kychenthal A, Lepore D, Lorenz B, Martinez-Castellanos MA, Özdek Ş, Ademola-Popoola D, Reynolds JD, Shah PK, Shapiro M, Stahl A, Toth C, Vinekar A, Visser L, Wallace DK, Wu WC, Zhao P, Zin A. International Classification of Retinopathy of Prematurity, Third Edition. Ophthalmology. 2021 Oct;128(10):e51-e68. doi: 10.1016/j.ophtha.2021.05.031. Epub 2021 Jul 8. PMID: 34247850; PMCID: PMC10979521.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10979521/
Reproduced for educational purposes.
Disease Severity
There are 5 stages of disease severity which are determined by the extent and the location of retinal damage.
Stage 1 is at the demarcation line that separates the vascular and avascular retina.
Stage 2 is at the ridge, which arises from the demarcation line and extends beyond the retina.
Stage 3 is characterized by extraretinal fibrovascular proliferation, which extends into the vitreous.
Stage 4 represents partial tractional retinal detachment and is subdivided into two subcategories:
Stage 4a is characterized by extrafoveal partial retinal detachment.
Stage 4b is characterized by foveal partial retinal detachment.
Stage 5 is characterized by total tractional retinal detachment.
Extent
Threshold disease is a term that describes ROP which has a high risk of retinal detachment if left untreated. This is defined by Stage 3 ROP with plus disease in Zone I or II. It must involve at least 5 contiguous clock hours or 8 total clock hours. Pre-threshold disease is characterized by Stage 3 ROP in Zone II or any ROP in Zone I.
Progression
Aggressive ROP (A-ROP) occurs when there is a rapid development of pathologic neovascularization and severe plus disease without the typical progression through the stages of ROP. This is no longer characterized by the location of disease, but instead by the progression and severity of disease, with notable vascular abnormalities.
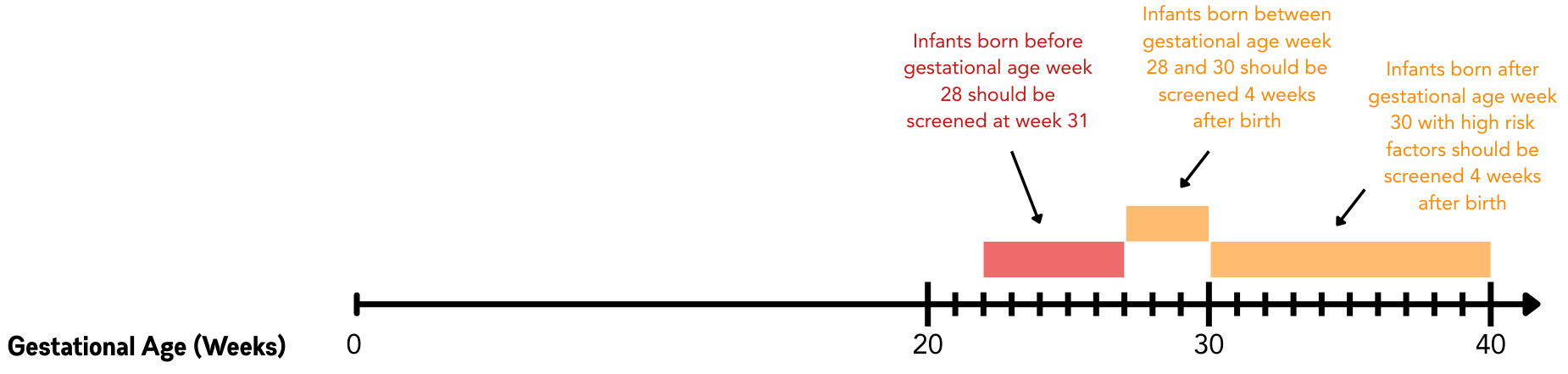
Risk Factors and Screening
Who To Screen
The most significant risk factors for ROP are premature birth (≤30 weeks gestational age) and low birth weight (≤1500 g). Other risk factors include:
Complicated clinical course
Oxygen (supplementation or fluctuation)
Slow postnatal growth
Increased altitude
Day length in early gestation
When To Screen
All infants who meet at least one of these criteria should be screened for ROP four weeks after birth or after 31 weeks postmenstrual age, whichever comes later.
Figure by Kevin E. Lai, M.D.
Table by Kevin E. Lai, M.D. and Ansam Qaddoumi, B.S., B.A.
How To Screen
ROP screening is performed on patients who meet the criteria above. These infants will need to have a fully dilated eye exam along with images to evaluate the full extent of their retinas. These include wide-field fundus photography, OCT, fluorescein angiography, and a B-scan if there is no clear view on the dilated fundus exam.
When To Stop Screening
ROP screening examinations can be discontinued once the retina has become fully vascularized, postmenstrual age is greater than 45 weeks with pre-threshold disease, Zone III has been vascularized without previous ROP in Zones I or II, or the disease has fully regressed. If patients have been treated with anti-VEGF injections, they should be followed up until at least 65 weeks postmenstrual age.
Treatment and Outcomes
Current treatments include laser photocoagulation therapy and anti-VEGF injections. Laser photocoagulation is recommended for any stage ROP with plus disease in Zone I, Stage 3 ROP without plus disease in Zone I, or Stage 2 or 3 ROP with plus disease in Zone II. Anti-VEGF injection therapy has shown benefits in Stage 3 ROP with plus disease in Zone I. However, per the RAINBOW, FIREFLEYE, and BUTTERFLYE trials, anti-VEGF injections demonstrated similar efficacy to laser coagulation therapy for disease treatment. Any patients with threshold disease should be treated immediately. Patients with pre-threshold disease should be monitored closely and treated if they develop plus disease. 90% of ROP cases will resolve, but there is a risk of retinal detachment and subsequent blindness, so short- and long-term follow-up is necessary.
References
Basic and Clinical Science Course, Section 6: Pediatric Ophthalmology and Strabismus. 2025-2026 Edition. San Francisco: American Academy of Ophthalmology, 2025. 339-349.
Basic and Clinical Science Course, Section 12: Retina and Vitreous. 2025-2026 Edition. San Francisco: American Academy of Ophthalmology, 2025. 193-214.
Chiang, M. F., Quinn, G. E., Fielder, A. R., Ostmo, S. R., Chan, R. P., Berrocal, A., ... & Zin, A. (2021). International classification of retinopathy of prematurity. Ophthalmology, 128(10), e51-e68.
Download a copy of this coffee table book page excerpt for free!