To help increase the amount of helpful study content on this site, I’ve partnered with some medical students from East Tennessee State University! They are being mentored by one of my former ophthalmology residents, Dr. Brent Aebi. The posts are primarily authored by the medical student, and reviewed/edited by myself and Dr. Aebi.
This post about corneal iron lines was written by Emily Rhoton, BS.
What Are Corneal Iron Lines?
Corneal iron lines are asymptomatic, benign physical exam findings that are thought to be caused by ferritin-bound iron or hemosiderin granules within the basal epithelial cells of the cornea (1). They appear as brown/yellow rings or lines within the epithelial cornea on slit lamp exam. Although benign in themselves, they can clue ophthalmologists in on possible pathological processes affecting other areas of the eye.
Why Do They Form?
Although no one truly knows the exact etiology behind corneal iron lines, there are a few hypotheses that you should be aware of:
Tear Pooling Hypothesis (1, 2)
Iron exists in tears, making it easy to be deposited in corneal areas of tear stagnation and pooling.Basal-Cell-Migration Theory (1, 3)
Basal epithelial cells migrate towards the center of the cornea, slowing where the cells originating cranially and caudally meet. Extracellular pigment would increase as neighboring cells divide, thus increasing iron line appearances with age.Tear Desiccation Hypothesis (1, 4)
Iron deposits in areas with tear film instability. Iron is left behind when tears are evaporated, leaving a higher concentration of iron in these places.Senescent Basal Cell Hypothesis (1, 4)
Less cell turnover means more iron accumulation.
Types of Corneal Iron Lines and Associated Conditions
There are four common types of corneal iron lines, each associated with a certain condition or pathology.
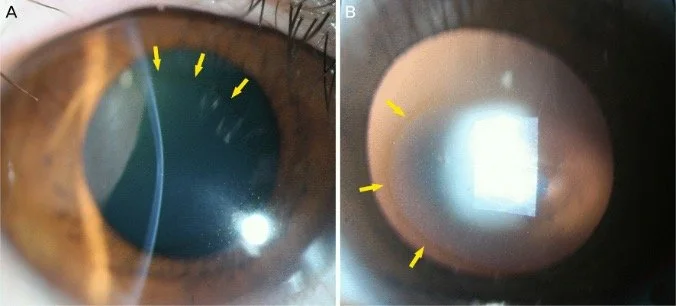
Fleischer Ring (1, 5)
Circumference around base of cone in keratoconus
Supports tear pooling hypothesis since iron is distributed around base of cone
Could also support epithelial cell migration due to corneal curvature altering migration path
Figure 1. Fleischer ring in keratoconus (6)
Figure 2: Hudson-Stähli Line (6)
Hudson-Stähli Line (1, 5)
Horizontal line in the lower third of the cornea (interpalpebral space)
Associated with normal aging or dry eye
Supports tear pooling hypothesis due to “blink line” formation where tear stagnation is common
Also supports senescent basal cell hypothesis due to formation in aging population, where cell turnover is decreased
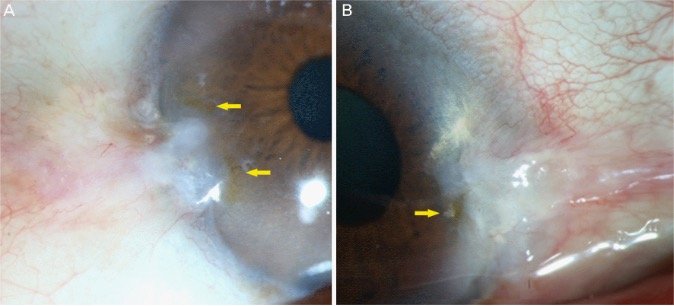
Figure 3: Stocker Line (6)
Stocker Line (1, 5)
Associated with pterygia
Vertical brown line on edge anterior to pterygium, often where the pterygium is stable
Supports tear desiccation hypothesis due to dry zones created by pterygia
May also support basal cell migration due to pterygia altering epithelial migration
Figure 4: Ferry Line (7)
Ferry Line (1, 5)
Golden brown line that appears anterior to filtering bleb
Occurs post-surgical glaucoma interventions with the creation of a filtration bleb, often with direct correlation to height of bleb
Supports tear desiccation hypothesis by elevation from bleb, leading to localized dryness
Could also support tear pooling hypothesis due to stagnation around bleb elevation
Other Corneal Iron Lines
There are also some less commonly known iron lines discussed here:
Baum Line
Usually seen in association with Salzmann’s nodular degeneration
Appears adjacent to stromal scar or elevated lesion (8)
Waring Line
Generally appears as a stellate pattern at middle/lower third corneal junction
Develops in approximately 80% of radial keratotomy (specifically RK) patients (9, 10)
Corneal iron lines can also occur after other keratorefractive surgeries, but they are not technically referred to as “Waring Lines”
Iron Overload ≠ Corneal Iron Lines
It is important to notice that none of the corneal iron lines are associated with systemic iron overload. This is a common misconception among new learners and patients.
There are two iron-overload condition that you should be aware of for ocular involvement: siderosis bulbi and hereditary hemochromatosis.
Siderosis Bulbi
This condition is caused by an iron-containing foreign body, which can be very toxic and vision-threatening. It will not present as a corneal iron line, but rather with rust-colored deposits with metallic foreign body on B-scan (11) The patient may report a history of trauma and unilateral symptoms.
Hereditary Hemochromatosis
This genetic condition may cause systemic iron overload. It includes a triad of cirrhosis, diabetes, and skin hyperpigmentation (5). This will not cause corneal iron lines, but rather, it can cause microaneurysms in the retinal vessels, retinal hemorrhages, and macular edema (similar to the presentation of diabetic retinopathy).
Histopathology & Stains
Histopathologic features and associated stains are commonly tested board topics. Corneal iron lines present as brown granular pigment located intracellularly within basal epithelial cells (8). It usually has no associated stromal changes. Fleischer rings in the setting of keratoconus may have central stromal thinning with focal discontinuities in Bowman layer (12).
Perls’ Prussian blue stain can be used for visualization of corneal iron lines, highlighting the ferric iron as a blue color (12).
Figure 5. Perls Prussian blue stain in a corneal iron line (13)
Figure 6. Fleischer ring with Perls Prussian blue stain (13)
References
Loh A, Hadziahmetovic M, Dunaief JL. Iron homeostasis and eye disease. Biochim Biophys Acta. 2009;1790(7):637–649. doi:10.1016/j.bbagen.2008.11.001
Gass JDM. The Iron Lines of the Superficial Cornea: Hudson-Stahli Line, Stocker's Line and Fleischer's Ring. Arch Ophthalmol. 1964;71(3):348–358. doi:10.1001/archopht.1964.00970010364010
Rose G, Lavin M. The Hudson-Stahli line III: Observations on morphology, a critical review of aetiology and a unified theory for the formation of iron lines of the corneal epithelium. Eye 1, 475–479 (1987). https://doi.org/10.1038/eye.1987.71
Assil KK, Quantock AJ, Barrett AM, Schanzlin DJ. Corneal iron lines associated with the intrastromal corneal ring. Am J Ophthalmol. 1993;116(3):350-356. doi:10.1016/S0002-9394(14)71353-4
American Academy of Ophthalmology. Ocular manifestations of hemochromatosis and iron-overloaded states. EyeWiki. Updated February 14, 2024. Accessed July 15, 2025. https://eyewiki.org/Ocular_Manifestations_of_Hemochromatosis_and_Iron-Overloaded_States
Kang TS, Lee JJ, Choi SH. Corneal iron lines observed in the clinical practice. J Korean Ophthalmol Soc. 2016;57(6):881-890. doi:10.3341/jkos.2016.57.6.881
Flynn SB. Corneal Iron Lines. Ophthalmology OKAP and Board Review Series. San Francisco, CA: American Academy of Ophthalmology; January 20, 2020. Accessed July 22, 2025. https://www.aao.org/Assets/aedd828b-faef-4f40-ae19-353a68c04c42/637151444223030000/k30u-pdf?inline=1
Reinach NW, Baum J. A corneal pigmented line associated with Salzmann’s nodular degeneration. Am J Ophthalmol. 1981;91:677–678.
Basic and Clinical Science Course, Section 8: External Disease and Cornea. 2016–2017 ed. San Francisco, CA: American Academy of Ophthalmology; 2017:321-322.
Nayak MV, Sharma H, Kalra J, et al. A comprehensive review of lines in ophthalmology: the anterior segment. J Clin Ophthalmol Res. 2025;4(4):24. Published April 2025. Accessed August 3, 2025. https://journals.lww.com/jcor/fulltext/2025/04000/a_comprehensive_review_of_lines_in_ophthalmology__.24.aspx
Casini G, Sartini F, Loiudice P, Benini G, Menchini M. Ocular siderosis: a misdiagnosed cause of visual loss due to ferrous intraocular foreign bodies-epidemiology, pathogenesis, clinical signs, imaging and available treatment options. Doc Ophthalmol. 2021;142(2):133-152. doi:10.1007/s10633-020-09792-x
Basic and Clinical Science Course, Section 4: Ophthalmic Pathology and Intraocular Tumors. 2016–2017 ed. San Francisco, CA: American Academy of Ophthalmology; 2017:95-96.
Mamalis N. Cornea Pathology. Moran CORE – Ophthalmic Pathology. John A. Moran Eye Center, University of Utah. Published December 27, 2017. Accessed August 3, 2025. https://morancore.utah.edu/section-04-ophthalmic-pathology/cornea/